Understanding Vaginal Discharge: From Normal to Signs of Infection
Vaginal discharge serves as a guardian of women’s health, but changes in it may signal underlying issues. This article delves into the essence of vaginal discharge, common problems, and treatment options to help you better listen to your body’s signals.
What is Vaginal Discharge?
Vaginal discharge is a fluid secreted by the vaginal lining and surrounding glands, forming a natural part of the female reproductive system. Under normal circumstances, it appears clear or white, with a mild odor, and provides lubrication while maintaining vaginal health.
Average women produce about 1 to 4 milliliters of discharge daily. This is not only normal but also helps prevent infections. However, abnormalities in color, odor, texture, or volume—accompanied by itching, burning, or inflammation in the vaginal area—may indicate an infection.
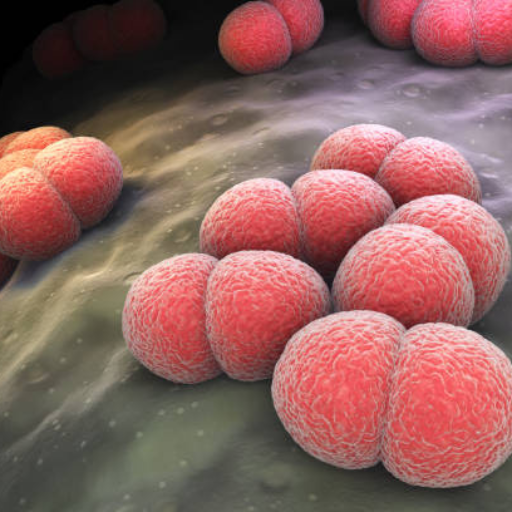
Common Types of Infections
- Trichomoniasis Vaginitis: Discharge appears yellow-green, foamy, thin, with a moldy or fishy odor.
- Candidal Vaginitis: Discharge resembles yellowish-white cottage cheese or curd-like.
- Bacterial Vaginosis: Discharge is grayish-white, thin, with a fishy smell.
Why Does Vaginal Discharge Increase?
An increase in vaginal discharge isn’t always concerning, but it’s important to identify the causes. Here are some common factors:
- Physiological Changes: Such as ovulation, pregnancy, breastfeeding, or sexual arousal, where hormonal shifts naturally boost secretion.
- Infections: Bacteria, fungi, or viruses (e.g., bacterial vaginosis, yeast infections, sexually transmitted diseases) often cause increases, along with itching, burning, or pain.
- Medication Effects: Certain hormones or antibiotics may trigger changes.
- Hormonal Imbalances: For instance, during menopause.
If the increase is accompanied by fever, pain, or other discomforts, seek medical attention promptly to diagnose the cause and receive appropriate treatment.
Common Treatments for Vaginitis
Treating vaginitis depends on the type of infection. Here are standard methods:
- Oral Antibiotics/Antifungals: Targeted at bacterial or fungal infections.
- Antibiotic/Antifungal Suppositories: Applied locally for direct effect.
- Antiviral drugs
6 Golden Rules to Prevent Vaginitis
- Stay Dry & Breathable: Wear cotton underwear and avoid tight pants. Ensure the private area is completely dry after bathing.
- Proper Cleaning: Always wipe from front to back after using the toilet. Avoid vaginal douching to maintain the natural pH balance.
- Menstrual Hygiene: Change sanitary pads or tampons every 2-4 hours to prevent bacterial growth.
- Healthy Diet: Reduce high-sugar foods (which trigger yeast growth) and take probiotics (like Lactobacillus) to maintain healthy flora.
- Safe Sex: Use condoms to reduce the risk of infections. It is recommended to urinate and clean externally after intercourse.
- Boost Immunity: Maintain a regular schedule and reduce stress. Strong immunity is the best defense against recurring infections.